The Biology of Stress and the Gut-Brain Revolution
Stress is a deeply biological event between your brain, hormones, and trillions of bacteria living in your gut.
In our modern world, "stress" has become a catch-all term for everything from a busy workday to profound burnout.
We often treat it as a purely emotional or psychological hurdle, something to be managed with willpower or a vacation.
However, science tells a different story: stress is a deeply biological event, rooted in complex feedback loops between your brain, your hormones, and—surprisingly—the trillions of bacteria living in your gut.
Understanding this biological reality is the first step toward true resilience. It explains why generic advice often fails and why personalised interventions, like those offered by the vivaBALANCE program, represent the future of mental wellness.
What is Stress? The Biological Mechanism
Biologically, stress is not just a feeling; it is a state of threatened homeostasis (balance). When your brain perceives a threat—whether a tiger in the wild or an overflowing inbox—it activates the Hypothalamic-Pituitary-Adrenal (HPA) axis.
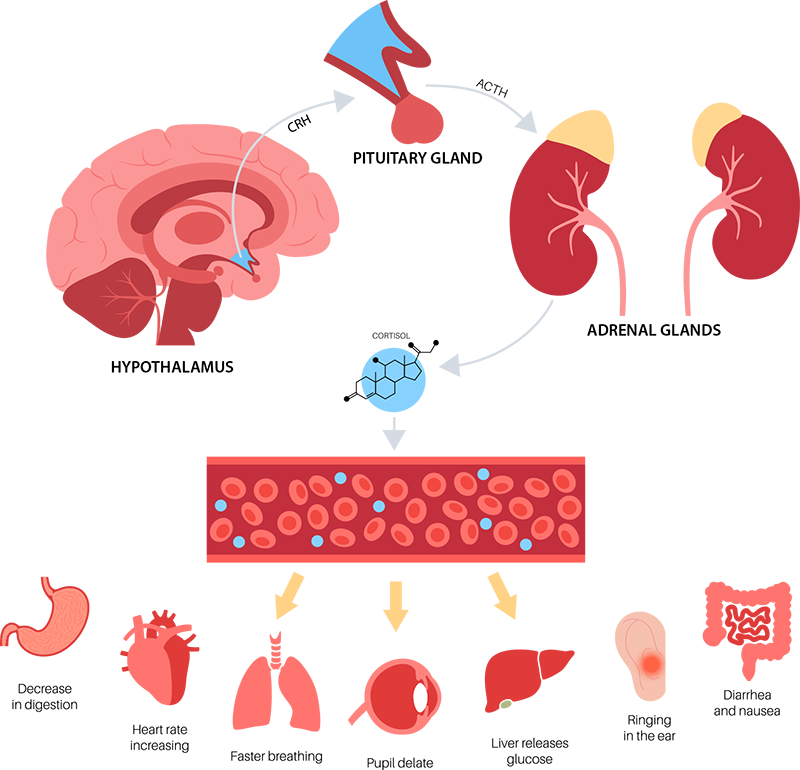
This activation triggers a cascade of events:
- The Alarm: The hypothalamus signals the pituitary gland, which then signals the adrenal glands.
- The Response: The adrenals flood your system with cortisol (the primary stress hormone) and catecholamines (like adrenaline).
- The Effect: Your heart rate spikes, glucose is dumped into the bloodstream for energy, and non-essential functions (like digestion and immune repair) are suppressed.
While this "fight or flight" mechanism is lifesaving in short bursts, chronic activation leads to "allostatic load" — the wear and tear on the body that accumulates over time [1]. Chronic cortisol exposure can degrade brain tissue, disrupt sleep, and exhaust your metabolic reserves.
Why We All Handle Stress Differently
Have you ever wondered why one person thrives under pressure while another crumbles? The answer lies in individual biology.
Your ability to manage stress is dictated by your genetic makeup and your physiological "set points." For example, variations in the genes regulating neurotransmitters like serotonin and dopamine can make some individuals naturally more anxious or less resilient to stressors [2]. Furthermore, your body’s ability to "shut off" the stress response is just as critical as its ability to turn it on. If your biological feedback loops are impaired—often due to inflammation or nutrient deficiencies—your cortisol levels remain elevated long after the threat has passed, leading to chronic anxiety and fatigue [3].
The Gut-Brain Connection: The Microbiome and Stress Resilience
The Gut-Brain Axis is a bidirectional communication highway linking your emotional and cognitive centres with peripheral intestinal functions. Your gut microbiome is a key regulator of this axis.
It influences your stress response in three critical ways:
- Neurotransmitter Production: Approximately 90% of the body’s serotonin (the "happiness" chemical) and a significant amount of GABA (the "calming" chemical) are produced or regulated in the gut. Dysbiosis (an imbalance of gut bacteria) can starve the brain of these critical mood-regulating chemicals [4].
- Inflammation Control: A "leaky" gut allows bacterial toxins to enter the bloodstream, triggering systemic inflammation. This inflammation can cross the blood-brain barrier, altering brain function and sensitizing the HPA axis, making you physically more prone to anxiety and depression [5].
- Vagus Nerve Signalling: Your gut bacteria communicate directly with the brain via the vagus nerve. Beneficial bacteria can send calming signals, while pathogenic bacteria can send signals that induce anxiety-like behaviours [6].
The Vicious Cycle: Metabolic Health and Stress
The stress-gut axis is inextricably linked to your metabolic health—how your body converts food into energy, regulates blood sugar, and manages fat stores. This forms a dangerous three-way feedback loop:
Stress Worsens Metabolism
When the HPA axis is chronically activated, high cortisol levels directly interfere with the function of insulin (the hormone that clears glucose from the blood). This can lead to insulin resistance, meaning cells ignore insulin's signal. The result is consistently high blood sugar, inflammation, and fat storage (especially visceral fat), which contributes to obesity and Type 2 Diabetes [8].
The Gut’s Metabolic Intervention (Good or Bad)
The gut microbiome acts as the critical mediator, determining whether this stress-metabolism cycle improves or spirals downward.
- Making it Better (A Healthy Gut): A diverse, balanced microbiome produces high levels of Short-Chain Fatty Acids (SCFAs), particularly butyrate. Butyrate is a foundational molecule that feeds gut cells, seals the intestinal barrier, and has been scientifically shown to improve insulin sensitivity and reduce inflammation throughout the body—directly offsetting the negative metabolic effects of stress [9].
- Making it Worse (A Dysbiotic Gut): Chronic stress hormones, such as catecholamines, can actually promote the growth of harmful bacteria and increase intestinal permeability [10]. An imbalanced gut releases toxins that flood the system, fuelling the low-grade, chronic inflammation that underpins both insulin resistance and heightened stress/anxiety responses [5].
This cycle is why stress management is impossible without addressing metabolic and gut function.
The vivaBALANCE Approach: Precision Health for Individual Resilience
The core issue with generic wellness advice is that everyone's stress, gut, and metabolic signature is different. The vivaBALANCE program, developed by vivaLAB, seeks to understand and optimise this unique relationship.
Multi-omic Diagnostic Testing
vivaBALANCE moves beyond generic blood work by leveraging sophisticated diagnostics:
- Metabolomic Testing: This provides a metabolic "fingerprint" by measuring chemical byproducts in the body. The test identifies key indicators of metabolic and stress dysfunction, such as Oxidative Stress Markers (cellular damage) and metabolites related to energy production.
- Microbiome Sequencing: This reveals the exact composition of the bacteria in your gut. For instance, it can pinpoint a low population of key butyrate producers (metabolic heroes) or a high level of pro-inflammatory bacterial metabolites.
- AI-Driven Personalisation: Uncovering the Root Cause
The true benefit of vivaBALANCE is its proprietary, AI-powered algorithm. This technology and science connects the dots between your different data streams—your gut bacteria profile, your metabolic markers, and your lifestyle inputs—a task impossible for a human to do manually.
- Example 1 (Stress): A consumer might have high stress due to high cortisol and low GABA-producing bacteria in their gut, which is a stress/gut problem.
- Example 2 (Metabolism): Another consumer might have poor energy and insulin resistance due to high stress, but the data reveals their gut is also poor at producing SCFAs—a stress/gut/metabolism problem.
By identifying the unique interplay between your HPA axis, inflammatory pathways, and metabolic markers, the program creates a truly bespoke Precision Nutrition Plan. This plan provides targeted supplements (including tailored psychobiotics), dietary advice, and lifestyle adjustments specifically designed to:
- Rebalance the Gut: Introduce strains or precursors that boost SCFA production to improve insulin sensitivity.
- Build Metabolic Resilience: Optimise energy pathways and reduce oxidative stress to mitigate the damaging effects of cortisol.
In essence, vivaBALANCE treats stress not as a singular mental state, but as a systemic, biological imbalance, offering a targeted solution where generic programs fail.
References (PubMed / PMC)
- Physiology, Stress Reaction. StatPearls [Internet]. (2024). [NCBI Bookshelf]
- Stress and Health: Psychological, Behavioral, and Biological Determinants. Annual Review of Clinical Psychology. (2008). [PMID: 17716044] / [PMC2568977]
- Neurobiological and Systemic Effects of Chronic Stress. Chronic Stress (Thousand Oaks). (2017). [PMID: 28856337] / [PMC5573220]
- The Gut-Brain Axis: Interactions between Enteric Microbiota, Central and Enteric Nervous Systems. Annals of Gastroenterology. (2015). [PMID: 25830558] / [PMC4367209]
- Stress in the Microbiome-Immune Crosstalk. Gut Microbes. (2024). [PMID: 38451021] / [PMC10950285]
- Stress & the gut-brain axis: Regulation by the microbiome. Neurobiology of Stress. (2017). [PMID: 29276734] / [PMC5736941]
- Gut Microbiota in Anxiety and Depression: Unveiling the Relationships and Management Options. Pharmaceuticals (Basel). (2023). [PMID: 37111281] / [PMC10146621]
- Signalling cognition: the gut microbiota and hypothalamic-pituitary-adrenal axis. Frontiers in Endocrinology. (2023). Describes cortisol's direct effect on gut and brain. [PMID: 38240409] / [PMC10803451]
- The gut-brain-metabolic axis: exploring the role of microbiota in insulin resistance and cognitive function. Frontiers in Microbiology. (2024). Discusses SCFA (Butyrate) improving insulin sensitivity. [PMID: 38859150] / [PMC11162357]
- Gut microbiota's effect on mental health: The gut-brain axis. Clinical and Translational Gastroenterology.(2017). Mentioned stress hormones influencing bacterial composition. [PMID: 28905814] / [PMC5641835]
Don't Miss Out on the Latest Insights
Sign up to our newsletter and stay in the loop with practical advice and discoveries in gut health, personalised wellness, and microbiome science.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply. By submitting, I agree to vivaLAB Privacy Policy. You can unsubscribe at any time.
You Might Also Like
Keep reading and discover more stories, tips, and insights that complement what you've just explored.
The traditional approach to men's wellness has focused on reactive treatment, but a new, proactive, and deeply personalised approach is revolutionising how men can achieve optimal health.
Dr Pennie Taylor dives into what’s really happening in women's bodies during perimenopause and menopause and how to thrive through The Change.
Explore Sleep’s importance, including its connections to lifestyle, metabolic health, and the gut microbiome. Evidence-based tips are provided to improve sleep and its health benefits.